World Antibiotic Awareness Week takes place on 12-18 November, with the 2018 European Antibiotic Awareness Day taking place on 15 November 2018. On these important dates, the health community raises awareness on Antimicrobial resistance (AMR), a growing threat around the world.
Resistance develops when microorganisms (including bacteria, viruses, fungi, and parasites) are exposed to drugs designed to harm their viability. The process of natural selection allows microorganisms to become resistant to a drug and to thrive despite drug exposure. Over time, the susceptible organisms are killed off, leaving behind only the resistant survivors. This renders common treatments ineffective and leaves patients vulnerable to spreading infection (WHO, 2018).
As infectious diseases make up a significant proportion of childhood illness, AMR is an important, evolving threat to children.
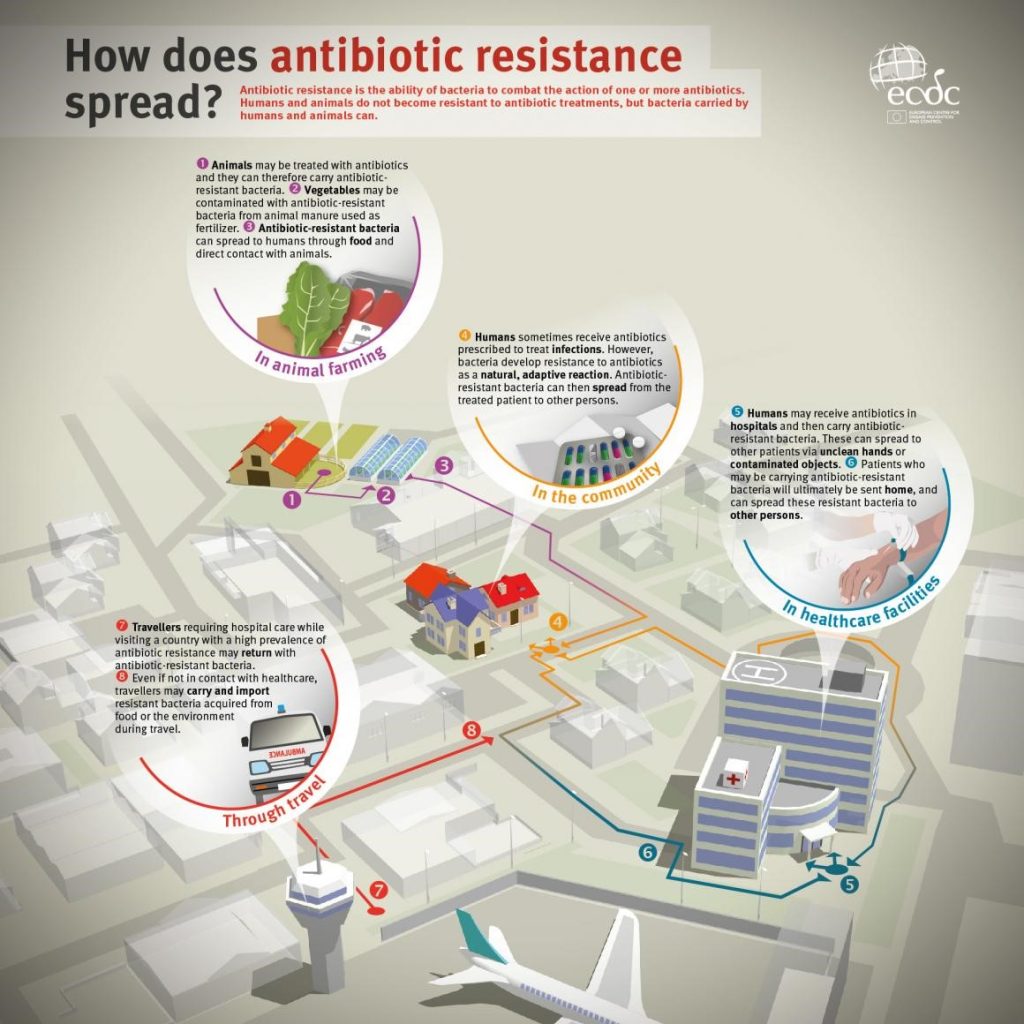
Antimicrobial resistance occurs through genetic changes in the microbe. Whilst this does happen naturally, it is accelerated by the misuse and overuse of antimicrobials. Once AMR has begun, it can then spread as shown below.
AMR in Europe: main threats and consequences
Data reported to the European Antimicrobial Resistance Surveillance Network (EARS-Net) for 2016 shows that AMR remains a significant public health and patient safety problem in Europe. Resistance rates vary across the region, with greater levels of resistance registered in southern and south-eastern Europe (ECDC, 2017). The CDDEP has put together a series of global and regional maps containing resistance data for individual pathogens.
The main danger of AMR is losing our ability to treat serious infections, which can have fatal consequences. AMR is an increasing child health concern as children are most susceptible to infectious diseases – they may have not yet developed immunity to some diseases, attend nurseries and playgroups with other children, and may be less attentive to hygiene. New-borns are most at risk from perinatally-acquired infection such as Group B Streptococcus (GBS) and E. Coli. Infants and children will therefore be one of the groups most affected by AMR.
Respiratory tract infections and urinary tract infections are both common in children, and AMR is increasing in organisms known to cause these. For example, more than one third of Klebsiella pneumoniae(causing urinary and respiratory tract infections) are resistant to at least one antibiotic group (ECDC, 2017). Escherichia coli, commonly responsible for urinary tract and other invasive infections, had shown increasing resistance to third generation cephalosporins between 2013 – 2016 across the EU. More than half of the isolates reported to EARS-Net were resistant to one or more antibiotic groups. Ten of 26 countries reporting Acinetobacter sp. resistance showed combined resistance in more than 50% of cases, leaving these patients with severely limited treatment options (ECDC, 2017).
A study in 2012 showed that across Europe Paediatricians did not correctly estimate the risks and benefits of antibiotic therapy for upper respiratory tract infections (Grossman et al, 2012). Education on this is needed to preserve our antibiotics to treat serious bacterial infections.
Likewise, drug resistant tuberculosis (TB) is a significant health challenge. There were 600,000 cases of new multi-drug resistant TB in 2016 (WHO). Healthcare providers must ensure they choose the correct treatment agent, dose and duration, plus educate their patients and their carers about the importance of treatment concordance (CDC).
AMR is also increasing in organisms known to cause hospital acquired infections, such as methicillin-resistant staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (ECDC, 2017). This puts already vulnerable hospital patients, including children, at increased risk.
This data clearly shows that AMR is leaving patients vulnerable to infections that may in the near future become unresponsive to current treatment options. Without effective antimicrobial therapy, these infectious diseases can be fatal. Immunocompromised patients, like those receiving chemotherapy or following organ transplants, will be particularly vulnerable. Post-operative and other hospital-acquired infections will be increasingly complex and difficult to treat.
A coordinated response is needed to tackle AMR. This must address all of the interconnected factors playing into AMR – isolated interventions will not be effective (WHO, 2018). Leading health organisations worldwide, including WHO, CDC, ECDC and IDSA, have repeatedly stressed the urgent need for improved surveillance of antimicrobial use and resistance patterns to evaluate evidence-based infection control and antimicrobial stewardship efforts.
The ECDC have launched a toolkit for the Antibiotic Awareness Day 2018 to support appropriate use of antibiotics in healthcare settings (EAAD, 2018). Reports show that aapproximately half of antibiotic prescribing in European hospitals is inappropriate: administration is often delayed, dosing or duration inappropriate, or the antibiotic chosen is from an excessively wide or (less commonly) too narrow spectrum. In addition, the antibiotic choice is often not reviewed or streamlined as soon as more information is available (ECDC, 2018).
Educational online courses on antibiotics and AMR offered by the WHO and ESPID (https://www.espid.org/default.aspx) aim to improve clinicians’ knowledge of, and competency in, AMR. Fighting antimicrobial resistance is also a core activity within ESCMID and GARDP. GARDPs neonatal sepsis programmes seek to provide an evidence base for the use of antibiotics in neonates with serious bacterial infections, as the currently available standard of care in many countries is increasingly becoming less effective due to antimicrobial resistance.
Education of the medical workforce is crucial. A European wide study on paediatricians’ attitudes and practice to antibiotic prescribing for upper respiratory tract infections found that 43.5% of respondents over-estimated the risks of not prescribing antibiotics, and over-estimated the clinical benefit of prescribing antibiotics, illustrating the need for further education and training (Grossman et al, 2012).
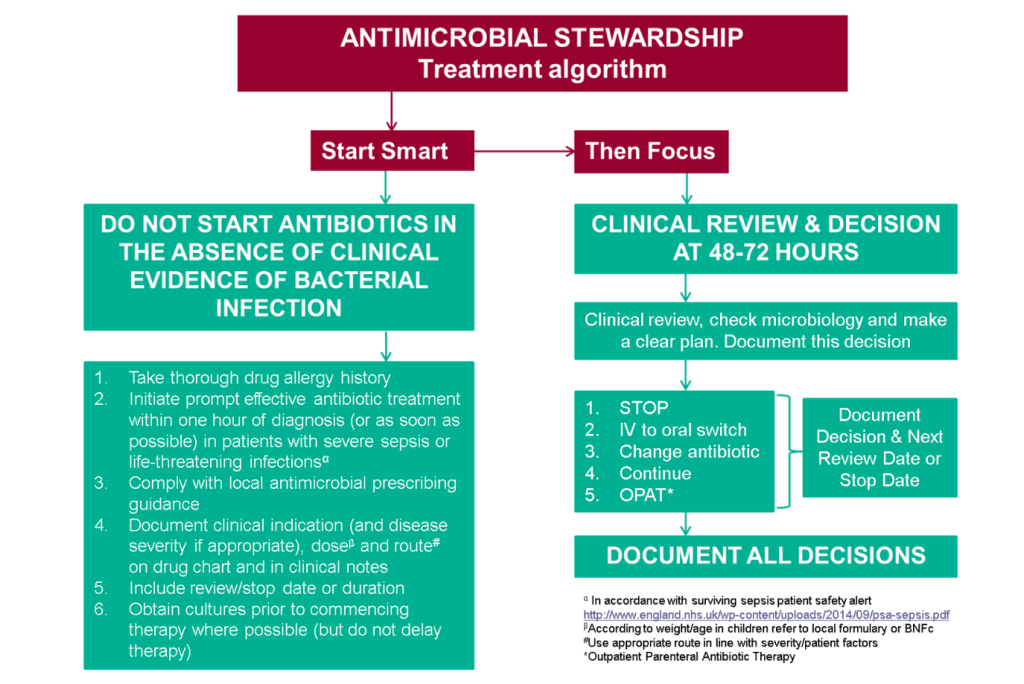
In the UK, a ‘Start Smart Then Focus’ initiative was launched by Public Heath England in 2015 to encourage appropriate antibiotic prescribing. Initiatives such as this encourage judicious evidence-based use of antimicrobials. ECDC found that hospitals that had implemented an antibiotic stewardship programme reduced inappropriate prescribing by 96%, length of stay and mortality by 65% and antibiotic resistance by 58% (ECDC, 2018).
Prevention policies are crucial to avoid AMR. These could include cohorting or isolating patients harbouring highly resistant organisms, screening for carriage of resistant organisms such as Carbepenamase-resistant Enterococci or MRSA, and the implementation of robust infection control policies to avoid hospital-acquired infections. Line care bundles to prevent central line sepsis have been successful in this regard.
Vaccination can go a long way in preventing disease before treatment is needed, thus reducing the potential for AMR. Conjugate pneumococcal vaccination has been shown to reduce rates of AMR amongst Streptococcus pneumoniae ssp. Childhood vaccination schedules cover may of the common infectious childhood diseases, and advocating vaccination and tackling vaccine hesitancy are therefore highly useful steps to prevent AMR.
The food and agricultural industry also has a part to play in tackling antibiotic misuse. Interventions restricting antibiotic use in food-producing animals can reduce AMR in microorganisms isolated from livestock by up to 39% (WHO, 2017). Healthy animals should only receive antibiotics to prevent disease if an outbreak in their population has been confirmed; and sick animals should receive targeted antimicrobial therapy, restricted to antimicrobials considered least important to human health (WHO, 2017). The EU banned the use of antibiotics for growth promotion in 2006. Similar initiatives should be considered worldwide.
Furthermore, AMR in low-income countries (LIC) presents an additional challenge. LIC deal with a significant infectious disease burden and healthcare systems are often less equipped to adapt to changes in resistance profiles. In particular multi-drug and extensively drug-resistant TB, as well as varying rates of resistence to antimalarial agents, are a growing problem in LIC. Only 30% of LIC have or are developing a plan to deal with AMR, compared to 80% of high-income countries (WHO, 2017). Again, children are one of the groups at most risk of infectious diseases, and therefore AMR is likely to present a particular threat to child health in LIC.
Finally, research must focuson new antimicrobials that offer therapeutic options to patients with highly-resistant organisms, as well as identify potential new vaccination strategies for the control of resistant pathogens. Such strategies have been the subject of important research into potential vaccines against Staphylococcus aureus, Group B Streptococci, and malaria. These areas should remain a research priority.
What we Recommend
EAP and Young EAP urge health care professionals to promote judicious and safe use of antimicrobials, and to advocate for other sectors to address antimicrobial misuse. The emergence of universally-resistant organisms, against which no current effective therapeutic options exist, raises the possibility of a return to a pre-antibiotic era. The effects of this could be devastating globally: it should be a worldwide priority to prevent this situation from happening.
Education of paediatricians across Europe and across primary, secondary and tertiary care should cover the risks and benefits of antibiotic prescribing. Paediatricians must ensure they are prescribing with clear clinical indications, and not over-estimating risks of not treating or benefits of treating (Grossman et al, 2012).
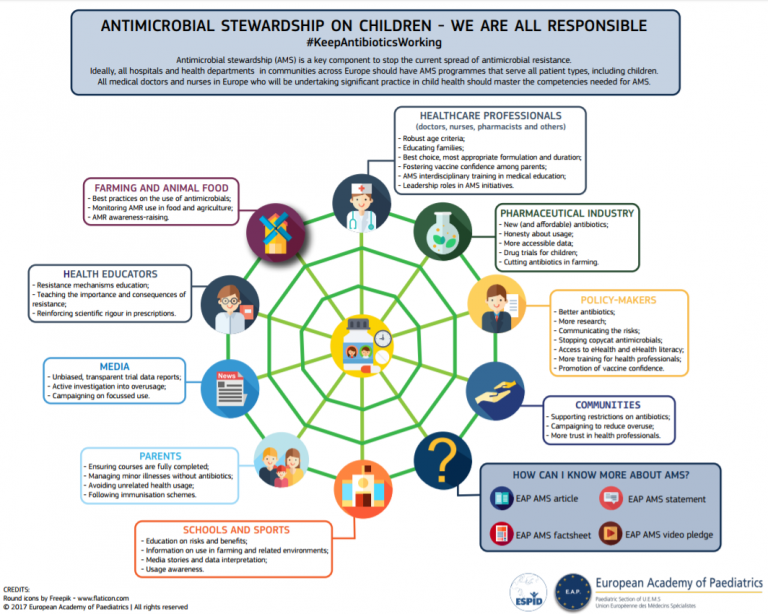
We also urge you to check our EAP infographic to learn more about the role of different societalgroups in tackling AMR by clicking on the image snippet below. Other useful EAP materials on AMR and Anti-Microbial Stewardship (AMS) include our factsheet with recommendations for health professionals and policy-makers.
Finally, EAP will take part in the World Antibiotics Awareness Week and Day activities this November, so be sure to check the EAP website and social media platforms for further content on AMR and AMS.
About the authors:
List of Authors
Lenneke Schrier is the European Junior Doctor Representative to the European Academy of Paediatrics, and the Chair of Young EAP. She is a 4th year paediatric trainee at the Leiden University Medical Center in the Netherlands.
Sian Copley is a 4th year resident from the UK working in the North East of England. Sian represents UK paediatric trainees within Young EAP, and paediatric trainees/Young EAP within the EAP Advocacy Group.
Paul Torpiano is a paediatric resident in Malta, and the Young EAP Representative for Migrant Health.
Daniela Kohlfürst is a member of Young ESPID (European Society for Paediatric Infectious Diseases) and Young EAP. She is a 4th year paediatric trainee at the Medizinisch Universitaet Graz, Austria.
Andreas Trobisch is member of Young EAP. He is a paediatric trainee at the University for Pediatric and Adolescent Medicine in Graz, Austria.
Hans Juergen Dornbusch is Chair of the EAP Vaccination Working Group. He is Associate Professor of Paediatrics at the University of Graz in Austria.
References

New ways to test high-risk medical devices.
Manufacturers of medical devices need to test their products before being allowed to market them. Specifically, they require clinical data showing their medical device is safe and efficient. In this context, the EU-funded CORE-MD project will translate expert scientific and clinical evidence on study designs for evaluating high-risk medical devices into advice for EU regulators. The project will propose how new trial designs can contribute and suggest ways to aggregate real-world data from medical device registries.
It will also conduct multidisciplinary workshops to propose a hierarchy of levels of evidence from clinical investigations, as well as educational and training objectives for all stakeholders, to build expertise in regulatory science in Europe. CORE–MD will translate expert scientific and clinical evidence on study designs for evaluating high-risk medical devices into advice for EU regulators, to achieve an appropriate balance between innovation, safety, and effectiveness. A unique collaboration between medical associations, regulatory agencies, notified bodies, academic institutions, patients’ groups, and health technology assessment agencies, will systematically review methodologies for the clinical investigation of high-risk medical devices, recommend how new trial designs can contribute, and advise on methods for aggregating real-world data from medical device registries with experience from clinical practice The consortium is led by the European Society of Cardiology and the European Federation of National Associations of Orthopaedics and Traumatology, and involves all 33 specialist medical associations that are members of the Biomedical Alliance in Europe.