YOUNG EAP BLOG | CREATING CONFIDENCE IN VACCINE
March 11, 2018
March 2018
How artificial intelligence can revolutionize medicine and pediatrics in the EU
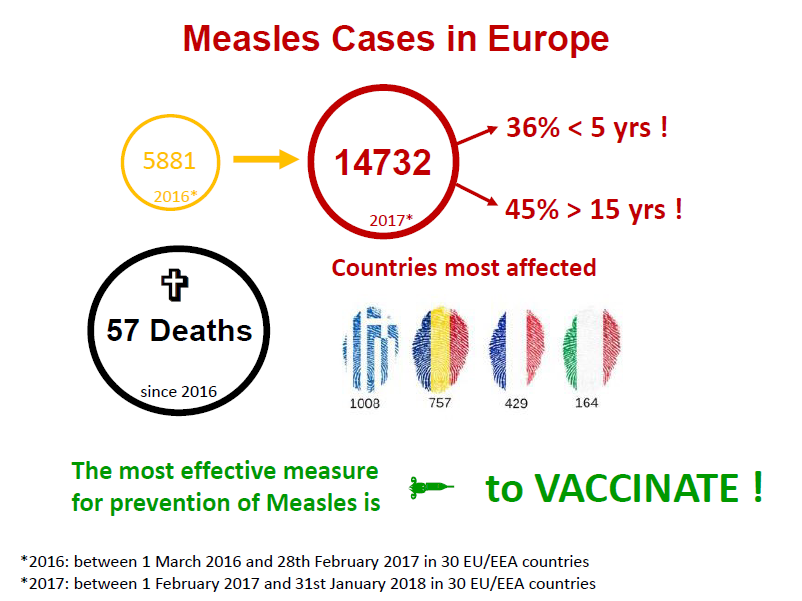
Across Europe we have been facing the problem of decreasing immunisation coverage that undermines the progress made towards eliminating specific infectious diseases, and allows vaccine-preventable disease to re-emerge. We need to explore the reasons behind this phenomenon, and to address them. Therefore, EAPRASnet, the practice-based research network within the European Academy of Paediatrics (EAP), is currently undertaking an EU-wide Vaccine Confidence Survey among parents, in collaboration with the London School of Hygiene and Tropical Medicine. The aim of the study is to assess parental behavior regarding immunization of their children, and to explore attitudes and beliefs regarding vaccine safety and efficacy.
Vaccine hesitant parents are parents who refuse or delay vaccines. Vaccine hesitancy is a complex challenge that requires a multifaceted approach with a strong, consistent message. The Strategic Advisory Group of Experts on immunization (SAGE), established by WHO, defined confidence, complacency and convenience as key factors that influence vaccine hesitancy. We know that the number of vaccine refusers who are absolutely non-responsive to any pro-vaccine arguments or actions has remained constantly small, whereas the group of vaccine-hesitant individuals is extensive and still growing. It is the latter group that may be open to solid, consistent, and evidence-based vaccine promotion.
Knowledge gaps, misconceptions and vaccine related myths threaten confidence in vaccines. Misconceptions spread quickly via the internet, propagated by sensationalist websites that fail to reference the sources behind their claims. The internet is a primary source of health information for many people, and about 42% of parents consult the internet for vaccine information. It is increasingly difficult for both parents and doctors to filter data obtained on the internet. The anti-vaccine lobby is often backed by powerful and wealthy individuals, not to mention a young generation that is able to use social media efficiently to get their messages across. Thus, websites opposing vaccines and presenting anecdotal reports as scientific data, often appear professional.
Mainstream media have also had a role in the propagation of vaccine misinformation. In 2015, a documentary shown on one of Denmark’s national television stations, described three previously healthy girls suffering from nausea, headache and abdominal pain after vaccination against Human Papilloma Virus (HPV). HPV immunisation rate in Denmark subsequently fell from over 90% to below 50 %. Meanwhile large studies have shown no evidence for a causal relation of the HPV vaccine with the symptoms described in the documentary. Unfortunately, the effect of misinformation lingers on despite these studies. In Japan, the anti-vaccine lobby used various media to present preliminary and unconfirmed data from a mouse study linking HPV vaccine to brain damage. This was intensified by online footage of adolescent girls apparently bound to wheelchairs and experiencing unexplained neurological phenomena after immunisation. This media distribution caused a drop of HPV vaccine coverage rates from 70% to less than 1%. In response, the EAP expressed its concerns, particularly about the negative position taken by government authorities. The most infamous case of widespread vaccine misinformation dates from 1998, when Andrew Wakefield published data linking the MMR vaccine to autism and inflammatory bowel disease. He later admitted having falsified data for this study, and was struck off the medical register. Numerous large studies and meta-analyses have disproven his claims, but even today, doctors regularly find themselves dealing with the uncertainty and mistrust his fraudulent research has spread. Psychological research has shown that addressing misconceptions is difficult, and even reading evidence refuting a myth can strengthen an individual’s belief in it. Various public health authorities like the European Centre for Disease Control (ECDC) have taken a responsibility to address these myths, and right the wrongs false research has caused. Mainstream media should understand their responsibility to provide the public with correct and solid evidence, and be aware of the potential public health disasters including increased child mortality that misinformation can lead to. Furthermore, health ministries should respond immediately to falsehoods spread via the media and warn the public about unfounded media reports, with the aim of limiting the damage caused. The vaccine confidence project was founded to monitor public confidence in immunisation programmes by building an information surveillance system for early detection of public concerns regarding vaccines and to provide tools for early response to ensure sustained confidence in vaccines and immunisation.
A declining supposed risk for acquiring vaccine-preventable disease and a lack of recognition for the potential morbidity and mortality of these illnesses also undermine immunisation programs. Ironically, these misconceptions are probably a result of the success of immunisation programs to control diseases. In contrast, parents focus on adverse effects of vaccinations that are much more apparent and distressing to them. The challenge here is to convince parents to protect their children from relatively uncommon diseases, while addressing their fears about side effects of immunisation. Studies have confirmed that the doctor’s advice is one of the most important predictors of vaccine acceptance. Therefore, a profound understanding of vaccine preventable diseases is necessary to counsel children, adolescents, parents and other adults adequately. Being able to answer their questions could prevent vaccine hesitancy and generate more confidence in vaccines. Thus, educating doctors on safety and efficacy of vaccinations is crucial in our opinion. Conflicting messages from different doctors will undermine the message that vaccines are ultimately safe and effective in protecting children. Emphasis on teaching knowledge about vaccinations should already be made at both undergraduate and postgraduate level, particularly for general practitioners, paediatricians and gynaecologists, obstetricians, as well as midwives and nurses. Online courses, like the ESPID wiser immunizer course, are very useful in this regard. Public information campaigns on TV, the internet and social media can be very effective in educating people. This should include addressing children and adolescents directly. The WHO has proposed tailoring immunisation programmes (TIP) to support health care professionals and public health authorities in closing immunity gaps. TIP focuses on the identification of populations that are susceptible to vaccine-preventable diseases, on identification of barriers and motivators to vaccination and on recommendations how to sustain vaccination. One barrier to vaccination could be the limited time medical professionals are able to dedicate for appropriate counselling. Adequate honoraria for vaccination counselling could help to ameliorate this drawback. Potential motivators to vaccination and possibilities for facilitating vaccinations include the implementation of electronic immunisation records, personal reminders via emails or messages to smartphones, and incentives for adherence to the immunization schedule.
Another option to increase vaccine uptake is mandatory vaccination as recently implemented in Italy and France. In the US 50 states have school entry requirements regarding childhood vaccines. Nonetheless, 47 states allow religious exemptions and 17 states allow personal belief/philosophical exemptions. In 2017 the CDC identified about 30,000 children whose parents refused vaccines for religious reasons. There is a risk that such systematic enforcement of vaccination schedules could be perceived as oppressive and a threat to children, thereby possibly strengthening the anti-vaccine lobby. Mandatory vaccination with the possibility to “opt-out” may eventually be a more acceptable solution.
We as Young EAP have placed the propagation of vaccine confidence as one of our priorities. As future paediatricians we feel that all doctors have the obligation to cultivate profound knowledge about vaccinations by counselling children, adolescents and their parents adequately. Therefore, we suggest that proper teaching of vaccinations and vaccine-preventable diseases be ensured within curricula of undergraduate medical and healthcare-related studies, but also to encourage training courses for health care professionals. We also emphasize the importance of educating children and adolescents, starting in early childhood. Finally, we urge that mainstream media networks and companies take it upon themselves to publish vaccine-related information with the utmost responsibility. Failing this, we believe it is the health authorities’ task to ensure early detection of public concerns regarding vaccines and to address them accordingly to ensure sustained vaccine confidence. The EAP is prepared to work with governments and media and share the extensive evidence demonstrating the effectives and safety of vaccines.
About the authors:
List of Authors
DANIELA KLOBASSA
DANIELA KLOBASSA is member of young espid (european society for paediatric infectious diseases) and young eap. She is a 4th year paediatric trainee at the Medizinisch Universitaet Graz in Austria.
PAUL TORPIANO
PAUL TORPIANO is member of young eap. He is a 4th year paediatric trainee at The Mater Dei Hospital in Malta.
RENSKE VAN VUGT
RENSKE VAN VUGT is a board member of the Dutch Junior Paediatric Society and member of young EAP. She is a 3rd year paediatric trainee at the Groningen University Medical Center in the Netherlands.
LENNEKE SCHRIER
LENNEKE SCHRIER is the european junior doctor representative to the European Academy of Paediatrics. She is a 4th year paediatric trainee at the Leiden University Medical Center in the Netherlands.
HANS JUERGEN DORNBUSCH
HANS JUERGEN DORNBUSCH is chair of the EAP vaccination working group. He is associate professor of paediatrics at the University of Graz in Austria.
ADAMOS HADJIPANAYIS
ADAMOS HADJIPANAYIS is the secretary general of the EAP. He is assistant professor of paediatrics at the Faculty of Medicine of the European University Cyprus.
